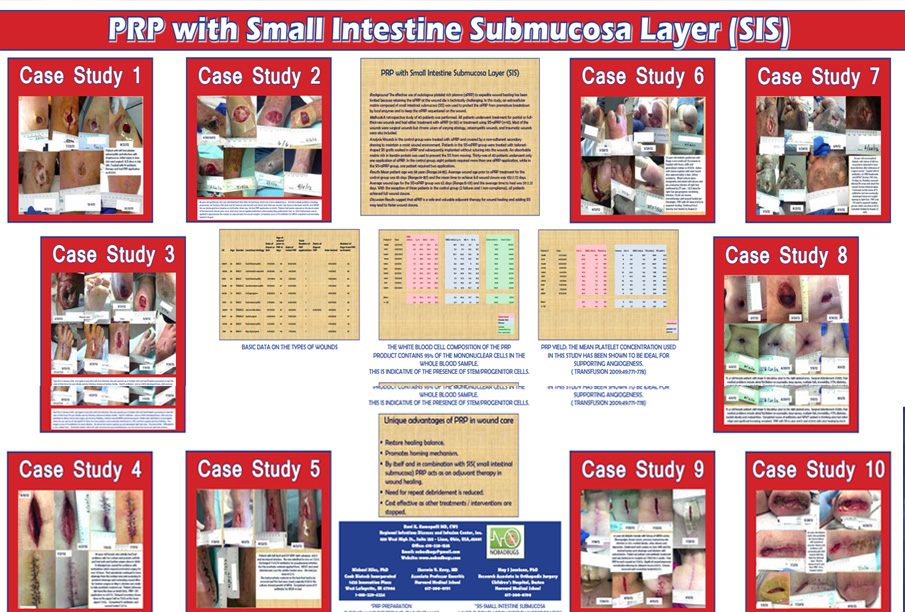
PRP with Small Intestine Submucosa Layer (SIS)
Background: The effective use of autologous platelet rich plasma (aPRP) to expedite wound healing has been limited because retaining the aPRP at the wound site is technically challenging. In this study, an extracellular matrix composed of small intestinal submucosa (SIS) was used to protect the aPRP from premature breakdown by local enzymes and to keep the aPRP sequestered on the wound. Methods: A retrospective study of 40 patients was performed. All patients underwent treatment for partial or full thickness wounds and had either treatment with aPRP (n=30) or treatment using SIS+aPRP (n=10). Most of the wounds were surgical wounds but chronic ulcers of varying etiology, osteomyelitis wounds, and traumatic wounds were also included. Analysis: Wounds in the control group were treated with aPRP and covered by a non-adherent secondary dressing to maintain a moist wound environment.
Patients in the SIS+aPRP group were treated with tailored shaped SIS grafts soaked in aPRP and subsequently implanted without suturing into the wounds. An absorbable matrix rich in keratin protein was used to prevent the SIS from moving. Thirty-one of 40 patients underwent only one application of aPRP. In the control group, eight patients required more than one aPRP application, while in the SIS+aPRP group, one patient required two applications. Results: Mean patient age was 58 years (Range:24-85). Average wound age prior to aPRP treatment for the control group was 83 days (Range:14-187) and the mean time to achieve full wound closure was 102±72 days. Average wound age for the SIS+aPRP group was 62 days (Range:15-131) and the average time to heal was 59±21 days. With the exception of three patients in the control group (2 failures and 1 non-compliance), all patients achieved full wound closure. Discussion: Results suggest that aPRP is a safe and valuable adjuvant therapy for wound healing and adding SIS may lead to faster wound closure
